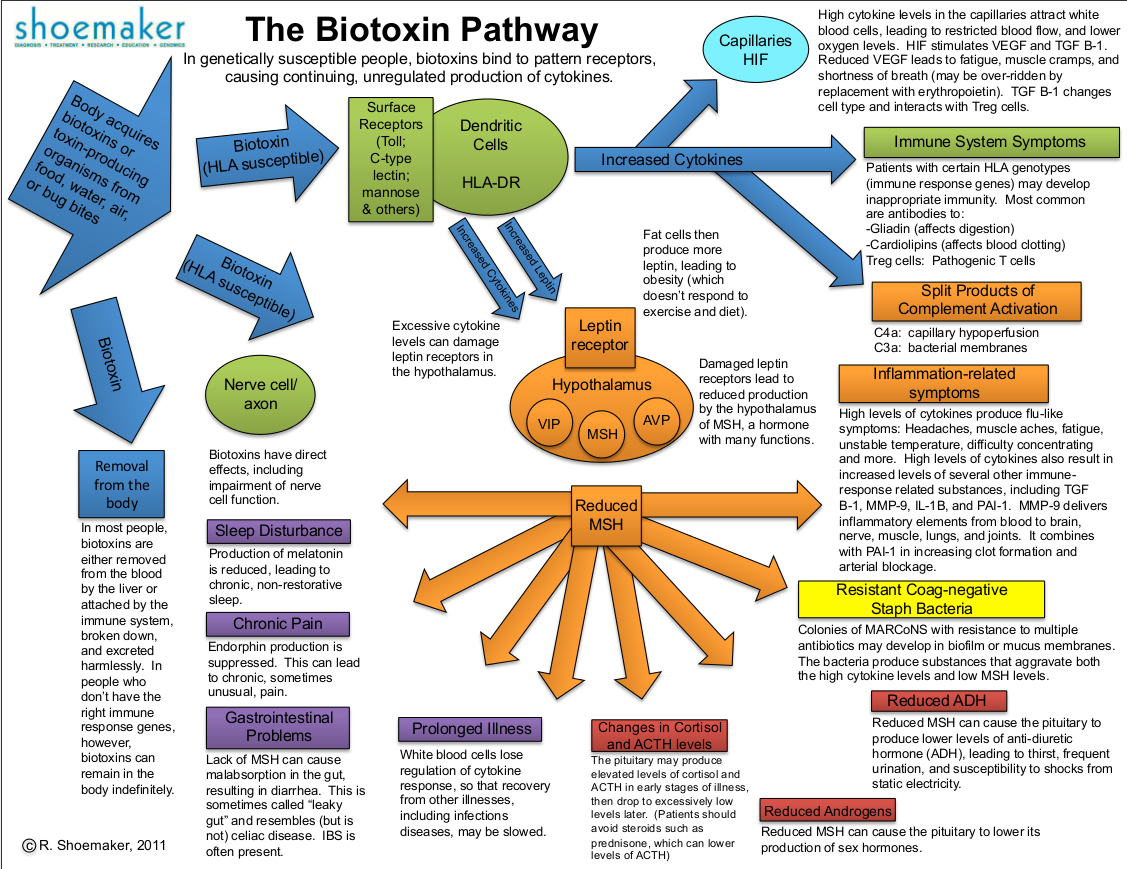
Schéma général de l'impact des biotoxines dans le corps (Shoemaker 2011)
--------------------------------------------------------------------------------------------------------------
- Biotoxines-pathways.jpg (702.37 Kio) Vu 12530 fois
Stage 1: Biotoxin EffectsIt all starts when a person is exposed to a biotoxin. In most people, the biotoxin is 'tagged' and identified by the body's immune system and is broken down and removed from the blood by the liver. However, some individuals do not have the immune response genes (HLA-DR genes) that are required to eventually form an antibody to a given foreign antigen. In these cases the biotoxins are not 'tagged' and remain in the body indefinitely, free to circulate and wreak havoc.
Once present in the body, the biotoxins begin to set off a complex cascade of biochemical events. The biotoxin binds to surface receptors (Toll receptors and many more) in nearly every kind of cell in the body. This recognition and binding of the biotoxin causes a continual upregulation of multiple inflammatory pathways, including production of cytokines, split product of complement, and TGF Beta-1. Biotoxins also directly affect nerve cell function, which is one of the reasons that the symptoms and visual contrast sensitivity (VCS) test are so useful in diagnosis.
Stage 2: Cytokine EffectsCytokines in turn bind to their receptors, causing release of MMP9 in blood. In the brain, cytokines bind to the leptin receptor, preventing its normal function in the hypothalamus. The blocked leptin receptor will no longer create the initiation of steps that lead to production of alpha melanocyte stimulating hormone (MSH). Elevated cytokines can produce many different symptoms including: headache, muscle ache, unstable temperature and difficulty concentrating. This problem is the disastrous effect of MSH deficiency. High levels of cytokines can also result in increased levels of important compounds such as I-1 and clotting factors as shown by a von Willebrand’s profile. Of importance in cardio vascular health, MMP-9 delivers inflammatory elements from the blood into sensitive tissues and can combine with PAI-1 to increase clot formation and arterial blockage.
Stage 3: Reduced VEGFThe elevated cytokine levels in the capillaries attract white blood cells, leading to restricted blood flow and lower oxygen levels in the tissues (we call this capillary hypoperfusion). Reduced VEGF leads to fatigue, muscle cramps and shortness of breath.
Stage 4: Immune System EffectsPatients with certain HLA genotypes (immunity related genes) may develop inappropriate immune responses which may include antibodies to: gliadin (gluten sensitivity), actin, anca (think ulcerative colitis), cardiolipins (affects blood clotting), and more. Most devastatingly of all, the complement system becomes chronically activated resulting in high levels of C4a.
Stage 5: Low MSHReduced MSH production results in yet another set of problems and symptoms. The production of melatonin is reduced which results in sleep problems. Endorphin production is suppressed which leads to chronic and sometimes unusual pain. Lack of MSH can cause malabsorption or 'leaky gut' which further weakens and deregulates the immune system. White blood cells eventually lose regulation of cytokine response so that opportunistic infections may occur or recovery from infections is slower.
Stage 6: Antibiotic Resistant Staph Bacteria
Reduced MSH also allows resistant staph (MARCoNS) to survive in biofilm on the mucous membranes. These bacteria further compound MSH deficiency and the problem by producing exotoxins A and B that cleave MSH, further decreasing the MSH levels. At this point, the downward spiral starts to perpetuate itself.
Stage 6: Pituitary Hormone EffectsReduced MSH can decrease pituitary production of antidiuretic hormone (ADH) which can lead to thirst, frequent urination, neurally-mediated hypotension (NMH), low blood volume, and electric shocks from static electricity. While sex hormone production is often down-regulated the pituitary may upregulate the production of cortisol and ACTH in the early stages of illness, then drop to abnormally low, or low-normal ranges later.
![bien [img]smile/thumb.gif[/img]](./images/smilies/thumb.gif)







 )
)